HAND CONDITIONS
Basal joint OSTEOARTHRITIS
Overview
This condition is a degeneration of cartilage in the joints at the base of the thumb, collectively called the basal joint. The main component of the basal joint is the thumb carpometacarpal (CMC), joint. This joint, which allows the thumb to pivot and swivel, can wear out even early in life.
Causes
This condition is caused by aging, repetitive motions, and wear and tear that occurs during normal use of the hand. It typically results from weakness of the volar beak ligament, which normally helps maintain joint stability. When this ligament weakens, the thumb can begin to move abnormally and the joint becomes irritated and inflamed. Gradually, the cartilage that lines the joint degenerates, allowing bone to rub directly against bone. As the CMC joint degenerates, other articulations of the basal joint can become affected.
Symptoms
The most common symptom is pain at the base of the thumb, especially when gripping or pinching. A grinding sensation may be felt when the thumb is moved. The thumb may also become weak and stiff. As the condition worsens, the joint may become deformed, and a bump may form where the thumb meets the wrist.
Diagnosis
The doctor will order x-rays of the wrist and hand to diagnose this condition. MRI or CT scans are usually not required.
Treatment
Treatment options include cortisone injections, non-steroidal anti-inflammatory medications, use of a splint or brace, exercise, and modification of daily activities. Surgery may be needed.
© Swarm Interactive, Inc.
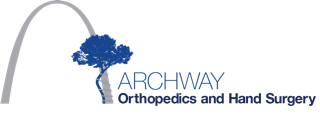
Boutonniere Deformity
Overview
This condition is a characteristic deformity of the finger in which the finger's middle joint, called the PIP joint, bends downward and the finger's end joint, called the DIP joint, hyperextends.
Causes
This condition is caused by an injury to the finger's extensor tendon, called the central slip. The central slip runs along the back of the finger and attaches to the middle phalanx at the PIP joint. This tendon is most often injured when an extended finger is forcefully flexed or dislocated toward the palm side of the hand, or by a laceration on the back of the finger near the PIP joint. The condition can also result from inflammatory arthritis or osteoarthritis, which can cause the tissues that stabilize the extensor mechanism to weaken and stretch.
Mechanism Of Deformity
When a central slip injury is not treated quickly and properly, the tissue stabilizing the accessory extensor tendons, called the lateral bands, can gradually weaken and allow the lateral bands to shift downward. This shift results in an imbalance in the forces that control the PIP and DIP joints, causing the finger to bend into a boutonniere deformity.
Symptoms
Common symptoms of acute central slip injury include swelling and tenderness over the top of the finger's middle joint. In severe injuries, or in injuries that are not treated quickly, the finger may bend into the characteristic boutonniere position. In an acute deformity, the PIP joint cannot be straightened on its own, but can be straightened using the other hand. In chronic deformity, the joint may become stiff and fixed in this bent position and is unable to be straightened even when using force.
Treatment
Treatment options may include a splint and hand therapy. For lacerations, severe joint dislocations, or chronic deformity, surgery is often required.
© Swarm Interactive, Inc.
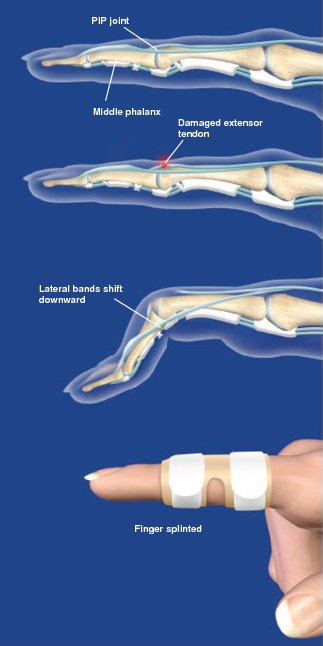
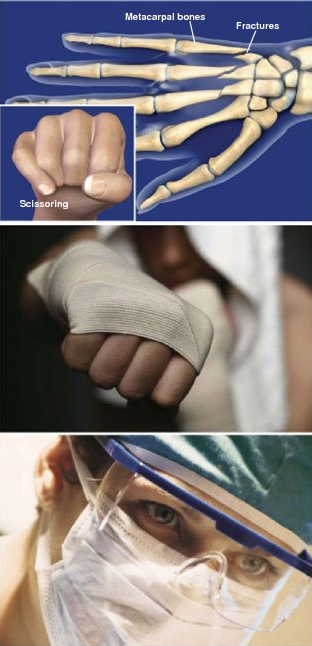
BOXER'S FRACTURE
Overview
A boxer's fracture is a break of the metacarpal of the little finger. The metacarpals are the long bones in the hand that connect the fingers to the wrist. A boxer's fracture refers to a break at the end of the bone nearest the knuckle, which is called the metacarpal neck.
Causes
This type of fracture most commonly occurs when someone punches a hard surface (or another person) with a closed fist. Since most people punch in a roundhouse fashion, the first point of boney contact in a punch is the little finger metacarpal bone. The force concentrates at the metacarpal neck, leading to a fracture. Ironically, this is a rare injury in boxers because they are trained to punch with even force over the entire hand, maximizing force and minimizing injury. A boxer's fracture can also occur when a person stumbles and tries to break his fall with a closed fist to the ground. Occasionally, direct trauma to the hand can also cause this injury.
Symptoms
Common symptoms include pain, tenderness, and swelling around the knuckle of the little finger. Bruising and loss of knuckle contour are also common, and extending the finger may be difficult. In severely displaced fractures, the fingers may overlap (or scissor) when they are flexed.
Treatment
Most boxer's fractures can be treated with a cast or brace to stabilize the fracture while it heals. If the knuckle is severely deformed, a procedure called a closed reduction may be needed to push the fracture back into proper position before casting. For severe displacement, finger scissoring, or multiple metacarpal fractures, surgery may be recommended.
© Swarm Interactive, Inc.
CARPAL TUNNEL SYNDROME
Overview
Pain, numbness and tingling in your hand may be from carpal tunnel syndrome. It happens when the area around the main nerve to your hand is too tight. The nerve is called the median nerve. And the small space in your wrist where it passes is called the carpal tunnel.
Causes and Risk Factors
Any crowding of the median nerve can cause this problem. Wrist injuries, diabetes and rheumatoid arthritis are causes. Pregnancy and conditions that cause your body to hold onto fluid may also cause it. Carpal tunnel syndrome is more common in women. You have a higher risk if your carpal tunnels are smaller than normal. Some think it's caused by repeated motions of the hand and fingers, especially a lot of typing at the computer. But evidence for that link is not clear.
Treatment
To get better, you may need to rest your hand and avoid doing the things that make your symptoms worse. Ice, wrist splints, medicine and injections may help. If they don't, surgery may be an option. Your healthcare provider can create a care plan that is right for your needs.
© Swarm Interactive, Inc.
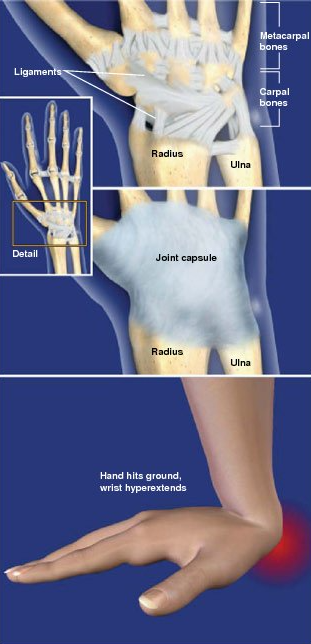
COLLES FRACTURES
Overview
Colles fracture is a break of one or both of the forearm bones (called the radius and ulna) that occurs just above the wrist. Although this type of injury can be caused by any strong force, Colles is most often associated with trying to break a forward fall.
Breaking A Fall
A person who falls forward will commonly try to break the fall by extending the hands and arms to reduce the impact of hitting the ground.
The Fracture
The combined pressure of hitting the ground and supporting a sudden load of body weight can cause the bones of the forearm to break just above the wrist. This is known as a buckle, or a Colles fracture.
Symptoms
Signs of a Colles fracture include pain and swelling just above the wrist and the inability to hold or lift heavy objects.
Treatment
Treatment ranges from simple immobilization to the use of a lightweight cast on the wrist. Recovery commonly lasts from six to twelve months. Severe fractures in which the bone is splintered or broken into many pieces may require pins or screws to hold the bones together while they heal.
© Swarm Interactive, Inc.
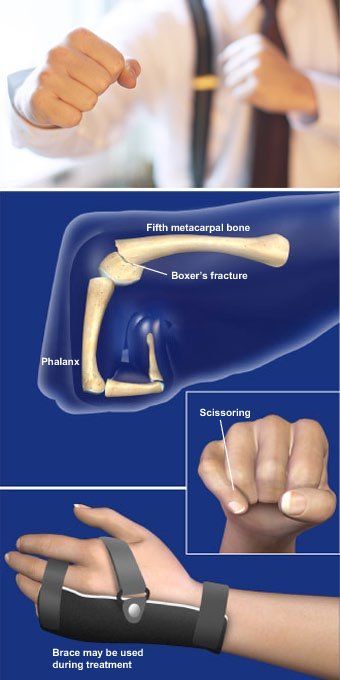
DE QUERVAIN’S TENOSYNOVITIS
Overview
This condition, also called stenosing tenosynovitis of the first dorsal compartment of the wrist, is an inflammation of the sheath that wraps around the tendons at the thumb side of the wrist.
Causes
This condition is caused by overuse, particularly from activities that require forceful gripping while flexing and extending the wrist. It is very common in new mothers (the result of grasping and lifting their babies) and from active gardeners who aggressively plant and weed. Occasionally, it is caused by direct trauma to the wrist. It is also more common in patients who have diabetes, rheumatoid arthritis, and other inflammatory conditions.
Symptoms
Symptoms can include pain and tenderness on the thumb side of the wrist when the wrist and thumb are moved. In some cases, a catching sensation may also occur. Gripping with the hand may be painful. Often, a firm nodule can be felt at the point of tenderness.
Treatment
Treatment options include rest, splinting of the wrist and thumb, and corticosteroid injections. Anti-inflammatory medications and a cold compress can also be used to relieve inflammation. If those treatment options are not successful, surgery may be needed.
© Swarm Interactive, Inc.
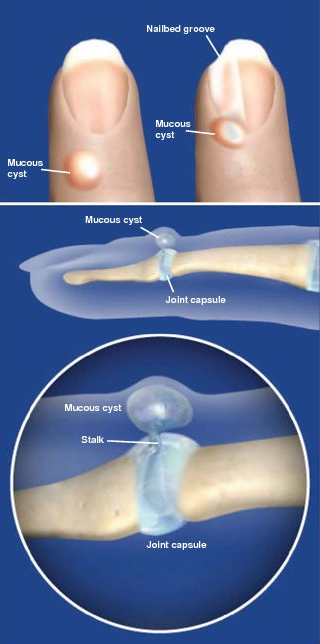
DIGITAL MUCOUS CYSTS
Overview
A mucous cyst is a small, fluid-filled sac that forms on the back of the finger near the base of the fingernail. It is a form of ganglion cyst that erupts from the capsule of the joint at the end of the finger, called the DIP joint. The cyst is attached to the joint capsule by a "stalk" that allows fluid to move into the cyst from the joint. Mucous cysts most commonly affect the index finger of the dominant hand.
Cause
Mucous cysts are caused by joint synovitis or arthritis at the DIP joint of the finger. It is believed that a weakness in the capsule leads to the formation of the cyst. Although cysts usually develop slowly, they can appear quite rapidly as well.
Symptoms
A mucous cyst appears as a visible bump under the skin. If it occurs near the nailbed, it may cause a groove to develop in the fingernail. A mucous cyst is typically not painful, but if it is repeatedly rubbed or bumped, the skin that covers the cyst may become irritated. Additionally, the arthritic or inflamed joint may cause discomfort. The skin that covers the cyst may become very thin and may rupture, resulting in drainage of a clear, jelly-like fluid. Because the cyst is connected to the joint, there is a risk of severe joint infection if the ruptured cyst becomes infected.
Diagnosis
Diagnosis of a mucous cyst involves x-rays, which are used to assess the condition of the joint and the severity of any underlying arthritis or synovitis. In many cases, bone spurs have formed on the top of the joint near the cyst.
Treatment
In many cases, mucous cysts do not need treatment. Small cysts that don't cause any problems may be treated with aspiration and a steroid medication. In more severe cases where the skin is thin and at risk of rupture, the cyst has become very large or painful, or the nail has become significantly deformed, surgical excision and joint debridement may be recommended.
© Swarm Interactive, Inc.
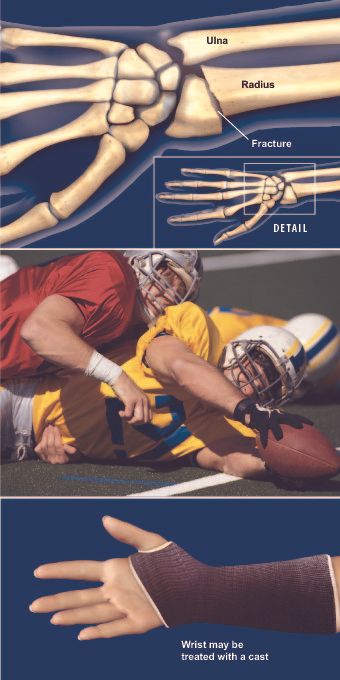
DISTAL RADIUS FRACTURE (BROKEN WRIST)
Overview
This condition is a break of the radius bone at the wrist. The radius is the larger of the two bones that connect the wrist to the elbow. The other bone is called the ulna. The radius supports the majority of forces at the wrist joint with its large joint surface. A fracture of the distal end of the radius - the end nearest the wrist -is one of the most common types of fractures. It may be part of a complex injury that involves other tissues, nerves and bones of the wrist.
Causes
A distal radius fracture is typically caused by direct trauma to the wrist. Common types of trauma include a fall on an outstretched hand, an automobile or bike accident, or a forceful blow to the wrist during a contact sport such as football.
Symptoms
Symptoms typically include pain, swelling, and tenderness at the wrist. The hand and wrist may be bruised and appear deformed. Moving the wrist may be difficult and painful. Mild numbness or tingling in the fingers may be present.
Treatment
Distal radius fractures can range from simple, clean breaks to severe fractures with multiple bone fragments. Treatment options, which vary depending on the type of injury, are designed to hold the broken radius in its correct position while it heals. If the fracture ends are out of alignment, the physician may need to perform a procedure called a closed reduction to realign them. The bones can then be stabilized with a cast, splint, or brace that may cover only the wrist and forearm or may extend to above the elbow. If the bones cannot be realigned with this method, surgery may be required.
© Swarm Interactive, Inc.
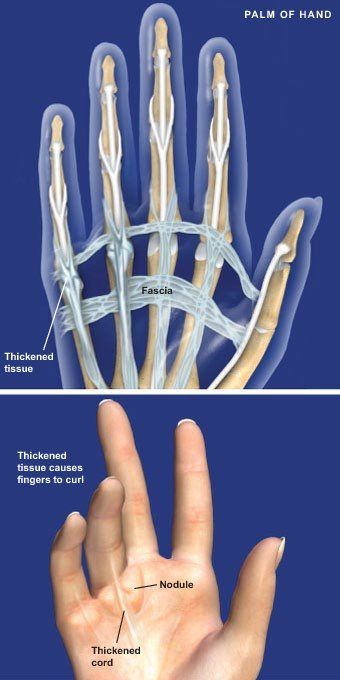
DUPUYTREN'S DISEASE
Overview
This condition is a thickening of the fascia on the palm of the hand. The fascia is a connective tissue located just beneath the skin of the palm and fingers. This thickened fascia can form lumps or nodules under the skin, or long thick cords of tissue that extend from the palm to the fingers. Often, this thickened tissue contracts. This causes one or more fingers to curl toward the palm. This is called a flexion contracture.
Dupuytren's Diathesis
Dupuytren's diathesis is a more aggressive form of Dupuytren's disease that occurs before the age of 40. It is associated with a strong family history, and affects both hands. A person who has Dupuytren's diathesis also commonly has other diseases of the fascia, such as nodules and contractures in the soles of the feet (called Ledderhose's disease) and curvature of the penis (called Peyronie's disease).
Overview
The exact cause of Dupuytren's disease is unknown. It most commonly affects white males of Northern European and Scandinavian descent over the age of 60. It is more prevalent in patients with diabetes. Smoking, lung disease, alcoholism, and use of anticonvulsant medication have been associated with Dupuytren's disease, but the relationship is unclear. Trauma to the hand may also play a role in its development.
Symptoms
The first symptom is a painless, firm nodule under the skin of the palm, most commonly in line with the ring or little fingers. As the disease progresses, the normal fascial bands may further thicken. They may form a cord that extends to one or more fingers. As the cord contracts, affected fingers begin to curl. They may not be able to be fully straightened.
Treatment
There is no treatment to cure or prevent Dupuytren's disease or its progression, but treatment may be used to relieve severe finger contracture. Treatment options include surgical excision of the thickened fascial tissue or an in-office needle release of the contracture. It can also be treated with an injection of an enzyme called collagenase. This enzyme weakens the contracted cord and allows it to be pulled and broken.
© Swarm Interactive, Inc.
FINGER DISLOCATION
Overview
If your finger is dislocated, that means a bone has been forced out of its normal position. It's a common, painful injury, and one that needs proper treatment.
Causes
Finger dislocations occur when your finger is forcefully jammed or bent past its normal range of motion. That can happen if you fall and try to catch yourself, or if you get hurt playing sports. In the fingers, most dislocations happen at the middle joint. In the thumbs, it's usually the joint at the thumb's base.
Symptoms
A dislocation hurts. Your finger may be bent at an odd angle, and it may swell. In most cases, you won't be able to bend or straighten it. Sometimes it's hard to tell a dislocation from a broken bone. A doctor can take images to decide.
Treatment
In many cases, a doctor can treat your dislocation without surgery. The bone is moved back into position, and your finger is supported with a splint. But sometimes, the bone is blocked by soft tissues. Or, the dislocation may have caused tissue damage. If so, you may need surgery to prevent long-term problems. Your healthcare provider can create a plan that's right for you.
© Swarm Interactive, Inc.
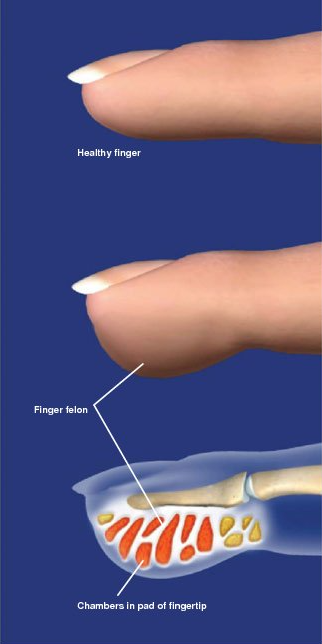
FINGER FELON
Overview
This condition is an abscess that forms within the pad of the fingertip. A felon can swell dramatically, leading to significant pain and sensitivity.
Anatomy
The pad of the fingertip is formed by a spongy layer of tissue made up of small chambers of fat.
How A Felon Forms
A felon forms when bacteria enter the pad of the fingertip through a puncture or cut. The bacteria invade the surrounding chambers in the pad of the fingertip, causing them to swell with fluid and eventually with pus.
Causes
Felons are commonly caused by puncture wounds from metal, glass, or other sharp objects. Diabetic blood draws at the fingertips can also cause a felon. The index finger and thumb are the most commonly affected digits.
Symptoms
Common symptoms can include severe, throbbing pain, swelling of the fingertip, and occasionally redness. In some cases the pressure inside the chambers builds and breaks through the skin, causing visible drainage.
Treatment
Felons require drainage of the pus from the chambers of the fingertip. Antibiotics and fingertip soaks are part of the complete treatment plan. A patient with a puncture wound or cut may also be given a tetanus shot.
© Swarm Interactive, Inc.
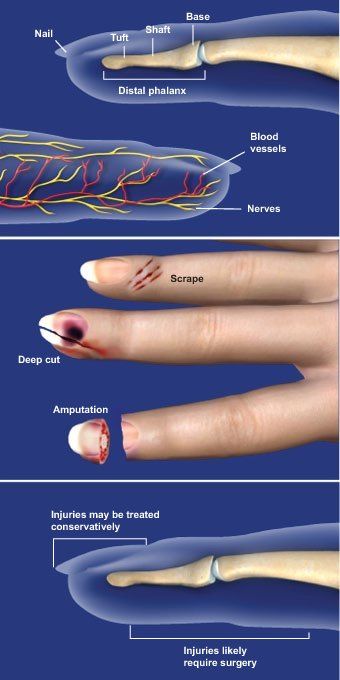
FINGERTIP INJURIES
Overview
Our fingers are often in harm's way, and our fingertips are prone to injury. A fingertip injury can involve skin, soft tissue, nerves and bone. It can involve the nail and the nailbed. These injuries can be serious, painful, and slow to heal. If you've injured your fingertip, you can take a few simple steps to minimize problems.
Injured, But Still Attached
If you've severely injured your fingertip but it's still attached, you should keep it clean and covered. If the skin is cut, try to help slow the bleeding with a clean wrap and some light pressure. Keep it raised, don't move it, and seek medical help.
Amputated
If your fingertip has been cut off, you need to preserve the amputated piece. A doctor may be able to reattach it. First, gently clean the amputated piece. You can use water, or you can use sterile saline solution. Protect it with a moist wrap. Put it in a watertight bag. Put that bag on ice. Don't let the fingertip have direct contact with the ice. This can damage the tissue. Get to a doctor as quickly as possible.
Treatment
Treatment options depend on how badly you've hurt your fingertip. You may need sutures or a splint. Your doctor may need to remove your nail, or make a hole in it to relieve pressure. You may need reconstructive surgery. You'll need to follow your doctor's instructions to make sure you avoid complications. Your healthcare provider can create a plan that's right for you.
© Swarm Interactive, Inc.
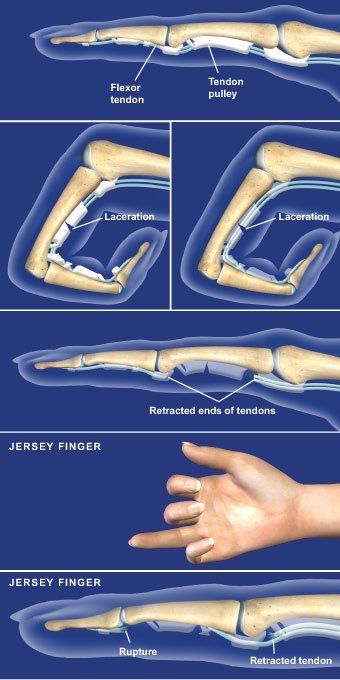
FLEXOR TENDON INJURIES
Overview
The flexor tendons of the hand are responsible for flexion of the fingers and thumb toward the palm. These long structures are connected to the flexor muscles in the forearm. An injury to one of these tendons can cause pain and inability to flex the finger or thumb and grasp with the hand. Common flexor tendon injuries include lacerations, ruptures and inflammation.
Lacerations
Cuts or penetrating trauma to the flexor tendons are frequently caused by accidents around the home or workplace. A laceration can sever a tendon, and can also injure other structures such as nerves and blood vessels that run parallel to the tendons. Commonly, a lacerated tendon retracts when severed, pulling away from the laceration site and slipping back through the tendon pulleys. Repairing a retracted tendon requires locating the ends and threading them back through the pulleys before they can be reattached.
Ruptures
Ruptures of the tendons are often caused by sports such as football or rugby, which require tackling. A common type of rupture, called a Jersey finger, is a rupture of the tendon at the fingertip.
Inflammation
Inflammation and spontaneous rupture of the flexor tendons can be caused by inflammatory conditions such as rheumatoid arthritis.
Symptoms
The most common symptoms for tendon laceration or rupture are pain and an inability to flex the finger. Swelling and bruising may also be present, but are less common. Symptoms for tendon inflammation can include pain, swelling, and limited range of motion.
Treatment
For flexor tendons that have been strained, treatment can include rest, anti-inflammatory medications, and often hand therapy. Tendons that have been cut or ruptured will require surgery to restore full use of the affected finger.
© Swarm Interactive, Inc.
FRACTURES OF THE HAND
(METACARPAL FRACTURES)
Overview
This condition is a fracture, or break, of one or more of the metacarpal bones of the hand. The fracture may be nondisplaced, in which the bones remain aligned, or displaced, in which the fractured ends shift out of alignment. Without proper treatment, the bones may not heal correctly. This can result in improper alignment of the fingers, leading to poor hand function.
Causes
This type of injury is most often caused by direct trauma to the hand. Punching another object, a sharp blow to the hand, a fall, or a twisting or crushing injury can all cause a metacarpal hand fracture. A common scenario is a young male injuring the metacarpal of the little finger during a fight. If the break occurs at end of the bone nearest the knuckle, this is called a boxer's fracture.
Symptoms
Symptoms typically include pain, swelling, and tenderness involving the broken metacarpal. Additional symptoms may include bruising on the back of the hand and in the palm, a bump on the back of the hand, and an overlap, or scissoring, of the fingers when making a fist.
Treatment
The most common form of treatment is placing the hand in a cast while the bones heal. The fingers may also be taped together to prevent rotation of the fracture in the cast. If the fractured ends are misaligned, the physician may perform a closed reduction, in which the bones are pushed back into their proper positions. If the bones cannot be acceptably realigned with this technique, or if there is scissoring of the fingers, surgery will likely be required.
© Swarm Interactive, Inc.
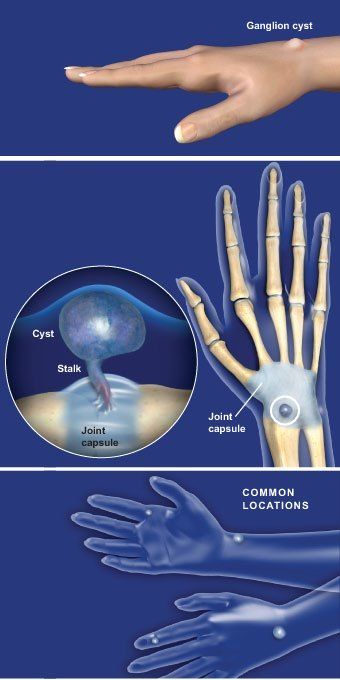
GANGLION CYSTS OF THE HAND
Overview
A ganglion cyst is a fluid-filled sac that forms as a herniation from a joint capsule or tendon sheath. The sac is attached to the joint or tendon sheath by a "stalk" that allows fluid to move into the pouch from the joint or sheath. The stalk functions as a valve and often limits fluid drainage out of the cyst, allowing the cyst to increase - but not decrease - in size. In some cases the stalk functions as a two-way valve, allowing fluid to travel in both directions. This can enable the cyst to increase and decrease in size based on activities.
Causes
The exact cause of ganglion cysts is unknown. They are believed to result from weakness of the joint capsule, ligaments or tendon sheath, which may be inherited or may be caused by arthritis, joint inflammation or trauma.
Where They Occur
Ganglion cysts can develop at any joint in the hand or wrist. They are most commonly found at the center of the back of the wrist. They are also commonly found on the palm side of the hand near the base of the fingers and the thumb side of the wrist, and on the back of the finger near the nail.
Symptoms
A ganglion cyst typically forms a firm bump under the skin. The bump may be large and obvious, or it may be very small and felt only with deep pressure. The cyst may increase in size during periods of increased activity, and then decrease in size with rest. Although most cysts do not cause pain, small cysts on the top of the hand can cause pain with wrist extension activities such as yoga or push-ups, and cysts on the palm side of the wrist may press painfully on the radial artery. Cysts in the fingers may cause pain when grasping objects.
Treatment
Not all cysts require treatment. Those that do not cause pain or limited motion can simply be observed - they may go away over time, especially in children. A painful or bothersome cyst can be drained with a needle (called aspiration), and a steroid can then be injected into the capsule or tendon sheath to decrease inflammation and decrease risk of recurrence. A cyst on the palm side of the wrist near the thumb often cannot be aspirated because of its proximity to the radial artery. For recurrent cysts or cysts on the palm side of the wrist or hand, surgical removal may be needed.
© Swarm Interactive, Inc.
KIENBOCK'S DISEASE
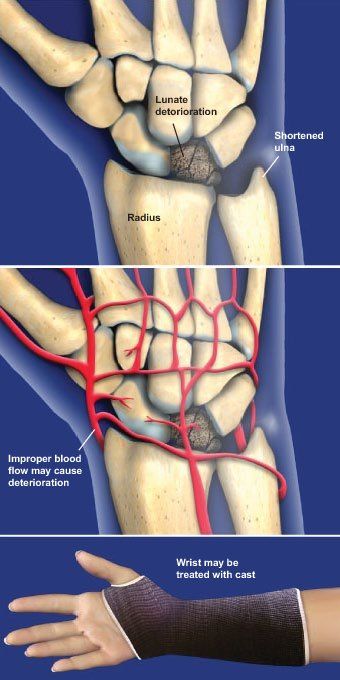
Overview
Kienbock's disease is the death and deterioration of the lunate, one of the small bones in the wrist. It usually occurs in young adults and causes wrist pain, weakness, and loss of motion.
Causes
The exact cause of Kienbock's disease is unknown. It may result from a compromise in the blood flow that supplies the lunate. Theories suggest that an increase of pressure within the lunate leads to congestion of the blood vessels that supply the bone, causing death of the bone cells. Some believe that it may be caused by trauma, although in many cases the disease cannot be tied to a specific traumatic event. A shortened ulna may also contribute to development of the disease, because a shortened ulna can cause the lunate to receive higher loads of pressure as the wrist is used.
Symptoms
Wrist pain, limited motion, and a weak grip are very common. Swelling and pain over the lunate on the top of the hand may also be present. The intensity of these symptoms may range from mild to severe.
Diagnosis
Kienbock's disease is diagnosed with x-rays of the wrist, which may show increased density of the lunate, cystic changes, fragmentation, bone collapse, or arthritis, depending on the stage of the disease. A bone scan or MRI may also be needed to confirm the diagnosis.
Treatment
The ideal treatment for Kienbock's disease is still debatable. Prolonged casting or bracing to rest the wrist and anti-inflammatory medications are usually the first recommendation for pain relief, but they do not necessarily halt disease progression. Surgery is usually recommended if conservative treatment does not resolve the pain. Surgical options may include shortening of the radius, vascularized bone grafts, or fusion of the carpal bones in the wrist.
© Swarm Interactive, Inc.
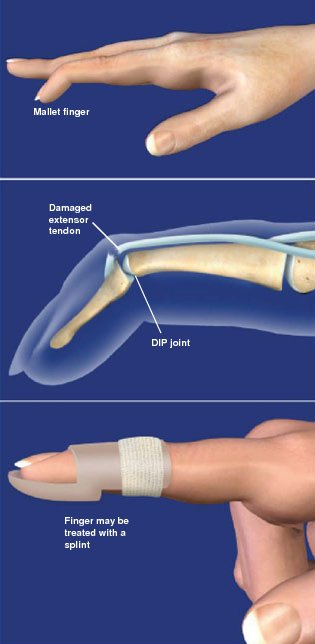
MALLET FINGER
Overview
This condition is an injury to the end of the extensor tendon that straightens the finger's end joint, called the DIP joint. It results in drooping of the fingertip, and prevents the finger from being straightened.
Causes
This condition is caused by an injury to the extensor tendon at the DIP joint. It can be caused by a laceration to the back of the finger, but most commonly results from direct trauma, often during sports when a ball strikes the extended finger. This can violently flex the tip of the finger, rupturing the extensor tendon. In some cases the tendon is pulled away from the bone, breaking a piece of bone from the tendon's attachment point. This type of injury is called a bony mallet finger.
Symptoms
The main symptom of this condition is a downward turning of the tip of a finger and an inability to straighten the affected finger. Other symptoms, which are most commonly associated with bony mallet finger, may include pain, swelling or tenderness.
Treatment
Mallet finger is commonly treated by placing the affected finger in a splint for at least eight to twelve weeks. If the bone fragment is very large or the joint is displaced, surgery may be recommended.
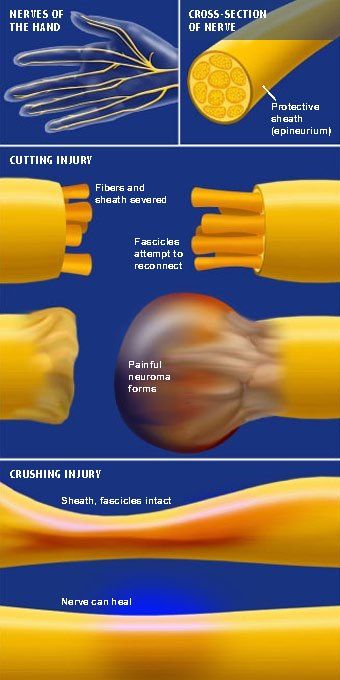
NERVE INJURIES OF THE HAND
Overview
Complex networks of nerves travel through your hands and fingers. If you injure a hand or a finger, you can damage these delicate nerves. Without proper care, a nerve injury can cause permanent problems.
Cutting Injuries
Cutting, crushing and stretching injuries can affect nerves. But different injuries can cause different problems. Each nerve is made up of a bundle of nerve fibers wrapped in a sheath. A cutting injury can slice through the sheath and the fibers. This lets the two ends pull apart. The nerve fibers may try to grow across the gap and reattach. But they don't always reconnect properly. Sometimes, they form a painful ball of nerve endings we call a "neuroma."
Crushing And Stretching Injuries
With crushing and stretching injuries, your nerve fibers may be stretched and torn. But the sheath around them may be intact. This can eventually let the fibers regrow and reconnect.
Symptoms
Symptoms depend on your injury. Some nerves carry sensory signals. Others control movement. Depending on which nerves are injured, you may feel numbness, weakness or pain.
Treatment
Some injured nerves can heal without surgery. But others need surgical help. If your nerve is severed, the ends may need to be reattached or placed in a guide so they can grow back together. You may also need physical therapy. Your healthcare provider can create a plan that's right for you.
© Swarm Interactive, Inc.
OSTEOARTHRITIS OF THE HAND
Overview
Osteoarthritis is the most common form of arthritis. It develops over time, often because of the wear and tear of daily activities.
Causes
Osteoarthritis is linked to a loss of cartilage. This is the tough, protective tissue that lines the ends of your bones. It helps your joints glide smoothly. But over time, your cartilage can weaken and wear away. Your joints become irritated and inflamed. Eventually, your bones begin to rub directly against each other.
Symptoms
In your hands, osteoarthritis can cause your joints to become swollen, stiff and painful. This can make it hard for you to do things like fasten buttons and tie your shoes. You may have swollen bumps called "cysts" that form in the joints nearest your fingernails.
Treatment
Osteoarthritis is treated with medications to help control your inflammation and relieve your pain. Wearing a splint may also help keep your joints from hurting. If these don't help, you may benefit from surgery. Your healthcare provider can create a plan that's right for you.
© Swarm Interactive, Inc.
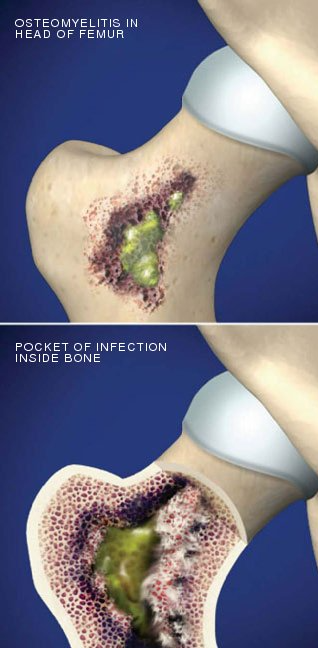
OSTEOMYELITIS
Overview
If you have an infection in a bone, you have osteomyelitis. It's a serious condition that can cause part of your bone to die. And, the infection can spread to other parts of your body.
Causes
A bone infection can be caused by a bacteria or a fungus. These germs can get into your body through a wound. They can get in during surgery. An infection can start in one place in your body and then move through your bloodstream into your bone. People who have diabetes or who are on dialysis have a higher risk for this type of infection. So do people who inject illegal drugs.
Symptoms
Osteomyelitis can cause pain at the site of the infection. You may have a fever and chills. You may feel bad all over. The skin near the infection may be red, warm and swollen. And, your legs and feet may swell. With time, the infection may cause an open sore to form in your skin.
Treatment
A doctor can treat your infection with surgery and with medications. Antibiotics may be given to you through an IV for several weeks. Usually, you need to be hospitalized. Your healthcare provider can create a care plan that is right for you.
© Swarm Interactive, Inc.
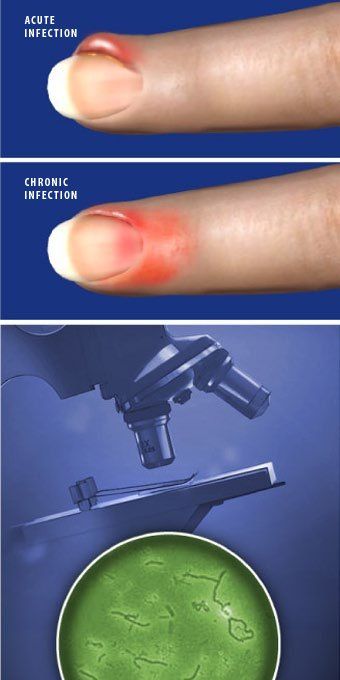
PARONYCHIA
Overview
This condition is an infection of the skin around the fingernail, usually at the side of the nail. Infections are usually mild, but may quickly increase in severity if not properly treated. Some infections may be chronic, and difficult to treat.
Acute Infections
Acute paronychial infections are caused by bacteria being pushed beneath the cuticle at the side or base of the fingernail. Once inside, the bacteria multiply and grow, first causing the surrounding tissue to become swollen and painful, then forming a pocket of pus. Common causes are hangnails, manicure instruments, nail biting, finger sucking, and trauma to the edge of the nail.
Chronic Infections
Chronic paronychial infections are most often caused by a fungus, in addition to bacteria. People whose hands are repeatedly exposed to water, such as dishwashers, bakers, bartenders, nurses, housekeepers and swimmers, are most at risk for this type of infection. Diabetics and people with a weakened immune system are also at risk.
Symptoms (Acute)
Symptoms of an acute paronychial infection include swelling, redness, throbbing, and tenderness at the nail fold. These infections are usually very painful and may have yellow or white drainage.
Symptoms (Chronic)
Symptoms for chronic infections include persistent redness, sponginess of the entire nail fold and repeated bouts of swelling and tenderness around the nail. Drainage is less typical in a chronic infection than in an acute infection. Symptoms are usually not as severe as acute infections, and may come and go depending on how often the area is exposed to water.
Treatment (Acute)
Most acute infections, especially cases in which an abcess has not yet formed, can be treated with warm water soaks and oral antibiotics. If pus has collected, it must be drained. Without treatment, the pus can spread to the opposite side of the nail, or even under the nail. If the infection progresses to this stage, part or all of the nail may need to be removed.
Treatment (Chronic)
Chronic infections may be treated with topical antibiotics, antifungal, or steroid medications. Oral antifungal or antibiotic medications may also be used. For more severe infections, part of the nail fold may need to be surgically removed to eradicate the infection. People with chronic infections are advised to avoid manicures, fingernail biting, finger sucking, and prolonged exposure to water.
© Swarm Interactive, Inc.
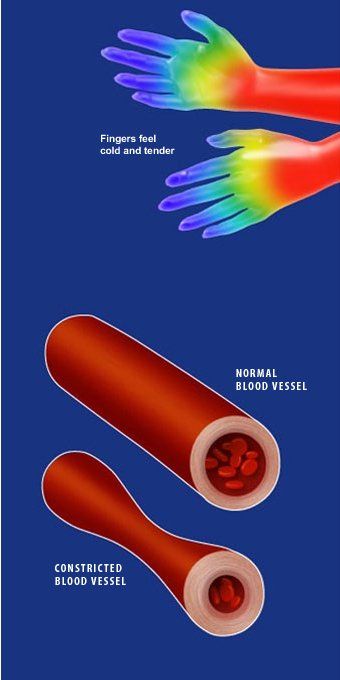
RAYNAUD'S PHENOMENON AND DISEASE
Overview
Raynaud's phenomenon is an exaggerated form of vasoconstriction - the body's natural response to cold and stress. It results from a spasm of the small arteries that supply blood to the fingers. This spasm temporarily decreases blood flow, resulting in cold, painful, and discolored fingers.
How It Occurs
Vasoconstriction is a normal process that is triggered when the body encounters a cold environment. The sympathetic nervous system causes the blood vessels in the extremities to constrict, keeping blood and warmth in the body's core. Raynaud's phenomenon is a misfiring of this process, causing abnormal vasoconstriction.
Causes
Raynaud's phenomenon can be caused by several medical conditions that affect the vascular system of the hands, including lupus and other connective tissue diseases, rheumatoid arthritis, arterial disease, and trauma. It can also be caused by smoking and by taking certain medications.
Raynaud's Disease
Raynaud's disease, a condition often confused with Raynaud's phenomenon, also results in vasoconstriction of the fingers. But while Raynaud's phenomenon is caused by an underlying medical condition, Raynaud's disease occurs without any underlying medical condition - its cause is not fully understood. Attacks of Raynaud's disease are triggered by cold and stress, and are most common in young women.
Symptoms
Symptoms of Raynaud's phenomenon and Raynaud's disease are similar. The most common symptom is hypersensitivity to cold and stress that results in a color change in the skin of the affected fingers. During an attack, the skin of the affected fingers typically turns white, then blue, then red - however, not all people experience all of these color changes, and not all people experience this particular sequence of colors. The affected area may also feel painful during the attack. An attack may be brief, lasting less than a minute, or it may last for several hours. Raynaud's disease typically affects both hands, but Raynaud's phenomenon typically affects only one. In severe cases, Raynaud's phenomenon can progress to cause thinning of the skin, ulcerations, and fingertip necrosis.
Diagnosis
It is important for a physician to differentiate between Raynaud's phenomenon and Raynaud's disease by studying a detailed medical history of the patient and the patient's symptoms. Blood tests and vascular studies may also be required. Once the condition has been diagnosed, the physician can determine the correct treatment plan.
Treatment
Treatment of Raynaud's phenomenon and Raynaud's disease typically begins with activity modification. Quitting smoking, avoiding cold environments, and wearing protective garments such as gloves or mittens will be recommended. Using biofeedback techniques to control the body's reaction to stress may also help control the condition. Medications may be used to dilate the blood vessels and decrease vasoconstriction. For severe cases, microvascular artery reconstruction or sympathetic nerve release may be required to restore normal blood flow to the fingers.
© Swarm Interactive, Inc.
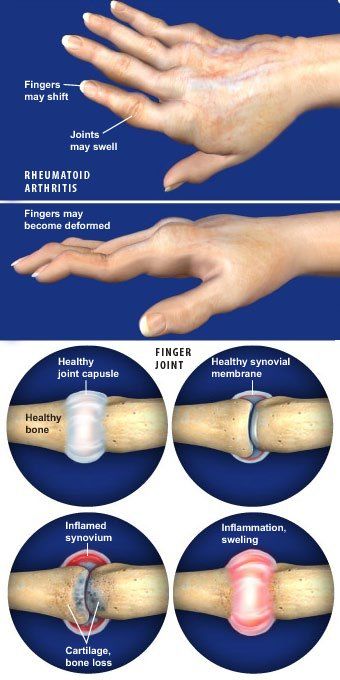
RHEUMATOID ARTHRITIS
Overview
Rheumatoid arthritis, a condition that can attack joints throughout the body, commonly affects the joints and surrounding tendons of the wrist and fingers. It can cause the joints to become swollen, painful and possibly deformed, interfering with normal hand function and significantly impacting a person’s quality of life.
Causes
The causes of RA are not fully understood. It is most likely caused by inherited genetic factors, but environmental factors may also play a role in triggering the condition. The disorder causes the immune system to attack the joints, causing the synovial membranes that surround the joints to become inflamed and swollen. This inflamed synovium leads to cartilage damage and bone loss around the joint.
Symptoms
Symptoms of rheumatoid arthritis in the hand can include stiffness (often worst in the morning), and pain and swelling in the joints, especially the joints at the base and middle of the fingers, the hand, and the wrist. The joints may become unstable and deformed. The knuckles may become inflamed, and the fingers may gradually lose their normal alignment. Often, the fingers angle away from the thumb. Additionally, the tendons of the wrist can become inflamed, and in severe cases may even rupture. Early tendon inflammation may result in a soft lump on the back of the hand or wrist. A person who has rheumatoid arthritis may develop other hand problems such as trigger finger, carpal tunnel syndrome, and boutenniere or swan-neck deformities of the fingers.
Treatment
Treatment options include anti-inflammatory medications, disease-modifying antirheumatic drugs, and a class of drugs called biological response modifiers (biologics for short). Splints or braces, exercise, and modification of daily activities may also be prescribed. Surgery may be needed when joint synovitis is not controlled by medications or the tendons of the hand and wrist become inflamed or weakened by the disease. Deformity of the fingers may also be treated with surgery to improve hand appearance and restore function.
© Swarm Interactive, Inc.
SCAPHOID FRACTURES
Overview
A scaphoid fracture, one of the most common types of wrist fractures, is a break in the scaphoid bone. The scaphoid, one of the most important bones in the wrist, has a limited blood supply. An improperly treated scaphoid fracture can result in significant wrist pain, arthritis, and loss of motion.
Anatomy
The wrist is made up of eight carpal bones and the ends of the radius and ulna. The carpal bones are arranged in two rows between the radius, ulna, and the metacarpals. The scaphoid spans between both rows of carpals, coordinating motion between the radius and the carpal bones.
Causes
The most common cause of a scaphoid fracture is a fall onto an outstretched hand, which causes the wrist to hyperextend and rotate toward the thumb. This position puts tremendous force at the scaphoid, and can cause it to bruise, crack, or break into two or more pieces. Other common causes for scaphoid fracture include automobile, motorcycle or biking accidents and forceful blows to the wrist.
Symptoms
Scaphoid fractures are often mistaken for wrist sprains because they have similar symptoms. Symptoms include pain, difficulty with wrist movement and grip weakness. A key symptom of scaphoid fracture is tenderness over the scaphoid bone at the base of the thumb, which may be felt on the back or the palmar side of the hand. Swelling and bruising may also occur on the palmar side of the wrist. If the fracture is displaced, a painful crunching, popping, or shifting sensation may be felt when the wrist is moved.
Diagnosis
A scaphoid fracture is a serious problem that may be confused with a wrist sprain. X-rays are needed to identify scaphoid fractures. However, some non-displaced scaphoid fractures may not be visible on x-rays until a few weeks after the injury, so x-rays may need to be repeated. A bone scan, MRI or CT scan may also be required.
Treatment
Treatment for scaphoid fractures depends on the fracture location and the presence of fracture displacement. Most nondisplaced scaphoid fractures will heal if treated in a cast for eight to twelve weeks. The cast usually includes the thumb, wrist, and forearm and may extend to or above the elbow. Some scaphoid fracture patterns do not heal well with cast treatment. For these fractures and displaced fractures, surgery will be necessary.
© Swarm Interactive, Inc.
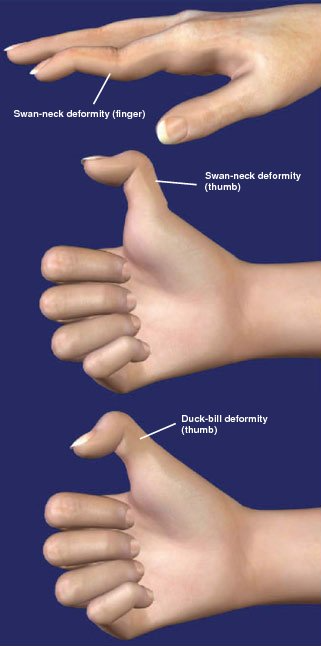
SWAN NECK DEFORMITY
Overview
This condition is a result of tendon imbalance in the finger or thumb. In the finger, it causes a characteristic deformity in which the middle finger joint (called the PIP joint) hyperextends, and the fingertip joint (called the DIP joint) bends downward. When viewed from the side, the finger looks like the outstretched neck of a swan.
In The Thumb
In the thumb, the condition causes the thumb tip joint (called the IP joint) to bend and the middle thumb joint (called the MCP joint) to hyperextend, resulting in the characteristic swan-neck appearance. If the IP joint bends but the MCP joint does not hyperextend, this is sometimes called a duck-bill thumb deformity.
Causes
This deformity is most commonly caused by rheumatoid arthritis, which can weaken or rupture the stabilizing tissues around the joints and can alter the joints' mechanics. It may also be caused by a hyperextension injury to the PIP joint, a mallet finger injury in a patient with loose ligaments, muscle imbalance, an improperly-healed finger fracture, or cerebral palsy.
Mechanism Of Deformity
In patients with rheumatoid arthritis (the most common scenario) swan-neck deformity is caused by synovitis and tissue inflammation of the PIP joint. The joint tissues weaken, allowing the joint to hyperextend and the lateral stabilizing tendons to shift above the joint axis. The flexor tendons become inflamed, causing the finger to flex at the MCP joint. This effectively shortens the extensor tendons, increasing the stress on the PIP joint and causing the DIP joint to flex.
Symptoms
Often, the only symptom of swan neck deformity is the deformity itself - hand function may not be affected. The tendons may snap as the finger is flexed. At times, this tendon snapping may become painful. As the deformity becomes more advanced, it may be difficult or impossible to flex the fingers into a fist, and arthritis in the fingers may cause joint pain and motion difficulty.
Treatment
Treatment options for swan-neck deformity vary depending on the severity of the symptoms. If the deformity is painless and does not affect function of the hand, treatment may not be needed. In other cases, specialized splints can prevent hyperextension and relieve snapping tendon discomfort. In more severe cases, surgery may be needed to stabilize or fuse the joint.
© Swarm Interactive, Inc.
THUMB ULNAR COLLATERAL LIGAMENT (UCL) INJURY
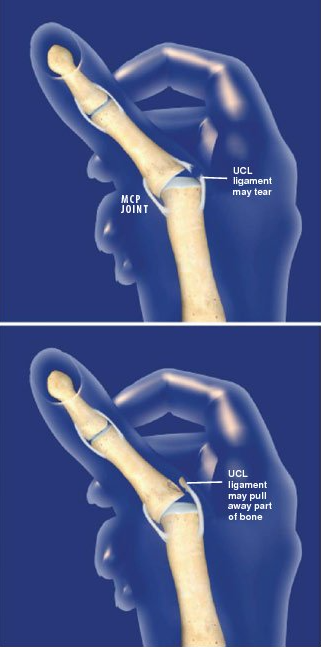
Overview
This condition, also called skier's thumb, is an acute sprain or tear of the ulnar collateral ligament (UCL) on the ulnar side of the metacarpal-phalangeal (MCP) joint of the thumb. A related condition, called gamekeeper's thumb, is a chronic injury that develops over time from repeated stretching of the UCL.
Causes
Injuries of the UCL occur when the extended thumb is bent radially away from the hand at the MCP joint. Common causes include a fall onto an outstretched hand, gripping the steering wheel during a car accident, and falling while holding a ski pole.
Symptoms
Symptoms typically include pain, swelling, and tenderness on the ulnar side of the thumb MCP joint. Pinching and gripping with the thumb may be difficult, and range of motion may be limited. In some cases, the ends of the torn ligament are held apart by a nearby tendon, forming a bump under the skin called a Stener lesion.
Diagnosis
A physician will diagnose a UCL injury by bending the thumb MCP joint away from the hand. Mild or partial tears are painful, but the joint will be stable. If the UCL is completely torn, the joint will be unstable. In severe cases, the joint capsule or volar plate (a thick, ligamentous band at the base of the joint) may also be damaged. X-rays will be required to check for a bone avulsion or fracture. An MRI may also be used to diagnose a displaced ligament.
Treatment
Partial tears and nondisplaced fractures are commonly treated by placing the thumb in a cast for 4 to 6 weeks. Complete tears and displaced fractures usually require surgery. Stener lesions always require surgery to avoid chronic pain and instability.
© Swarm Interactive, Inc.
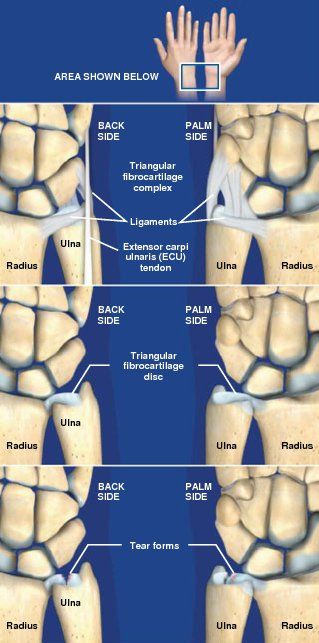
TRIANGULAR FIBROCARTILAGE COMPLEX (TFCC) TEARS
Overview
This condition is a degenerative or traumatic tear of one or more parts of the triangular fibrocartilage complex (TFCC), which stabilizes the ulna. The TFCC is composed of a group of ligaments that form connections between the radius, ulna and the carpal bones of the hand. At the center of these ligaments lies the most commonly injured structure, the triangular fibrocartilage disc, which is connected between the radius and the base of the ulnar styloid.
Causes
TFCC tears are often caused by degeneration through normal use of the wrist as we age. Overuse of the wrist with activities such as gardening or handling heavy luggage may further aggravate or tear the degenerative tissue. Traumatic tears may be caused by falling onto an outstretched hand, forceful twisting of the wrist and occasionally by a sharp blow to the outside of the wrist. The TFCC can also become torn during certain athletic activities, such as swinging a baseball bat, a tennis racquet or a golf club.
Symptoms
The primary symptom of a TFCC tear is pain on the ulnar side of the wrist. The pain may be accompanied by clicking, popping, catching or snapping when the wrist is rotated.
Diagnosis
Radiographs are used to evaluate the injured wrist. An MRI arthrogram, in which contrast dye is injected into the wrist joints during the MRI, may also be needed. If the physician cannot make a clear diagnosis using those methods, wrist arthroscopy may be used to look inside the wrist.
Treatment
Treatment options include rest, icing and anti-inflammatory medications for mild symptoms. A wrist brace, splint or cast may be used to prevent motion as the inflammation subsides. A corticosteroid injection may also be used to relieve inflammation. In severe cases with persistent pain or instability, surgery may be required to debride or repair the tear.
© Swarm Interactive, Inc.
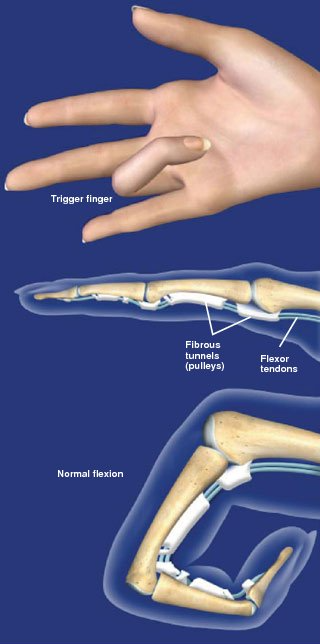
TRIGGER DIGIT
Overview
This common condition, also known as stenosing tenosynovitis, is a narrowing of a portion of the tendon sheath in the finger or thumb that interferes with normal finger movement. This condition most commonly affects the ring finger, but can affect any digit. It is more common in middle-aged women, but anyone can be affected, even newborns.
Causes
This condition may be caused by overuse or repetitive use of the hand. Normally, as a finger is bent and extended, the finger's flexor tendons glide smoothly through a series of fibrous tunnels in the finger and hand. Trigger digit results from a narrowing of the fibrous tunnel in the palm called the first annular (or A1) pulley.
How It Develops
Forceful flexion of the fingers causes stress at the A1 pulley and can lead to bunching of the fibers within one of the tendons. The tendon can swell and thicken, forming a bump called a nodule. The pulley also thickens and narrows, and the swollen tendon or nodule has trouble passing through the narrowed pulley during attempts to extend the finger from a flexed position.
Other Causes
Several medical conditions can increase a person's risk for trigger digit, including diabetes, rheumatoid arthritis, gout, renal disease, and other inflammatory conditions. In rare instances, trigger digit can also result from direct trauma over the A1 pulley.
Symptoms
The first symptom is typically a mild grating, crackling sensation at the metacarpal head when the finger is flexed or extended. This may be accompanied by pain. A bump may be felt beneath the skin on the palm at the base of the affected finger. The finger may be difficult to extend, and may click or catch as it is extended. Commonly, a person may wake up in the morning with the finger held in the flexed position. This catching may become severe, and, if left untreated, the finger can become permanently locked in the flexed position. Finger stiffness may also develop in chronic cases.
Treatment
Treatment options for very mild and early cases may include activity modification, splinting, or anti-inflammatories, but the results are unpredictable. Most commonly, a steroid injection to the flexor tendon sheath is recommended because of its high success rate. Diabetics and patients with rheumatoid arthritis may have less success with steroid injections. If injection does not relieve the symptoms, the next step is surgical release of the pulley. Hand therapy may be recommended after surgery or if finger stiffness is present.
© Swarm Interactive, Inc.
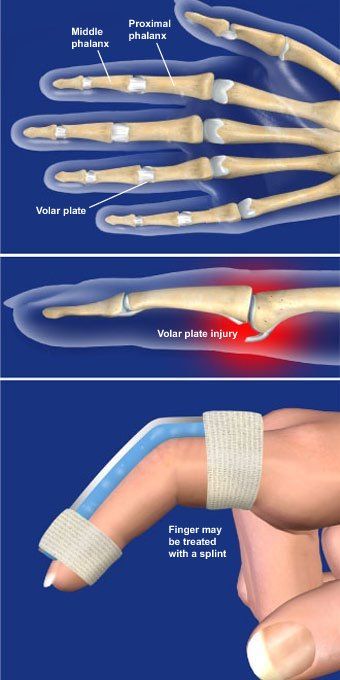
VOLAR PLATE INJURIES
Overview
This condition is a stretching or tearing of the volar plate, which can allow the finger to hyperextend and can interfere with normal hand function. The volar plate is a strong ligamentous structure on the underside of the finger at the point where the proximal and middle phalanx bones meet, called the proximal interphalangeal joint (or PIP joint). The volar plate keeps the finger from bending backwards at the PIP joint, and, together with the collateral ligaments, stabilizes the PIP joint from displacement.
Causes
Volar plate injuries can be caused by disease or trauma. Diseases such as rheumatoid arthritis can weaken and loosen the volar plate, leaving it susceptible to injury. Trauma to the finger, such as breaking a fall with an outstretched hand or catching a ball during athletic activity, can hyperextend or dislocate a finger and tear or rupture its volar plate and one or both of the collateral ligaments. In some cases, the bone at the attachment of the volar plate may fracture and be pulled away.
Symptoms
Symptoms of a volar plate injury include pain and swelling at the joint, tenderness on the palmar side of the joint, and joint instability. If the finger is dislocated, it may be noticeably out of alignment.
Treatment
Most volar plate injuries can be treated with a flexed finger splint, followed by finger motion exercises and hand therapy. If the joint is unstable or a significant fracture has occurred, surgery will be required.
© Swarm Interactive, Inc.
WRIST SPRAIN
Overview
When your wrist is bent too far, this can injure bands of tissue called "ligaments." Ligaments connect the bones of your hand to each other. They also connect the bones of your hand to the bones of your forearm.
Causes
You can sprain a wrist by trying to catch yourself when you fall. Your hand bends backward too far. This hurts your ligaments. Most wrist sprains involve the scapholunate ligament.
Symptoms
A wrist sprain can cause pain and swelling. Your skin may bruise. Your wrist may pop when you move it.
Treatment
A mild sprain may get better with rest and ice. Wrapping it and keeping it raised may help. A moderate sprain may need a splint. A severe sprain may need surgery. Your healthcare provider can create a care plan that is right for your needs.
© Swarm Interactive, Inc.